Otosclerosis
What Are The Risk Factors, Diagnosis and Treatments?
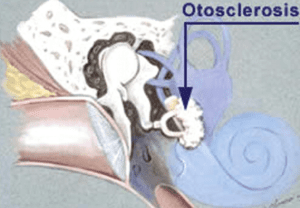
With normal hearing, sound enters the ear canal (external ear), vibrates the ear drum and the sound is conducted by the middle ear bones (malleus, incus and stapes) to the cochlear (inner ear) where it is turned into an electrical signal for the brain.
Otosclerosis or Otospongiosis as it is also known, is a condition in which there’s abnormal bone growth inside the middle ear reducing how sound is transmitted from the eardrum to the cochlear. In otosclerosis, the stapes (“stirrup” bone) begins to fuse with the surrounding bone, eventually becoming fixed so it cannot move. This means sound is no longer transmitted into the inner ear efficiently.
Why this happens is still unclear, but scientists think it could be related to a previous measles infection, stress fractures to the bony tissue surrounding the inner ear, or immune disorders. Otosclerosis also tends to run in families.
It may also have to do with the interaction among three different immune-system cells known as cytokines. Researchers believe that the proper balance of these three substances is necessary for healthy bone remodeling and that an imbalance in their levels could cause the kind of abnormal remodeling that occurs in otosclerosis.
Pathophysiology of Otosclerosis
Generally, bone remodelling occurs at a rate of 10% per year throughout skeletal regions. However, a normal otic capsule has very little bone remodelling, only 0.13% per year.
But bone remodelling within the otic capsule is increased in the patients with Otosclerosis. This leads to the accumulation of bone deposits that damage audiological structures and worsen normal sound transmission.
Abnormal bone remodelling occurs in three phases
- Otospongiosis phase – It represents an increase in both osteoclast activity and microvascularity.
- Transitional phase – It begins with deposits of spongy bone by osteoblasts in areas of previous bone reabsorption.
- Otosclerosis phase – In this phase, spongy bone deposits develop into the dense bone that narrows the microcirculation developed in the Otospongiosis phase.
What are the symptoms of otosclerosis?
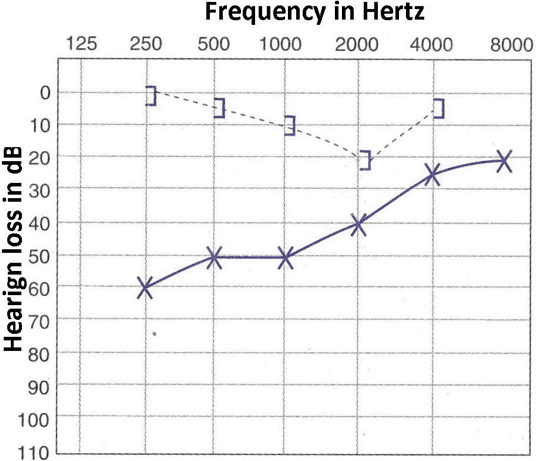
Hearing loss, the most frequently reported symptom of otosclerosis, usually starts in one ear and then moves to the other. This loss may appear very gradually. Many people with otosclerosis first notice that they are unable to hear low-pitched sounds or can’t hear a whisper.
Some people may also experience dizziness, balance problems, or tinnitus. Tinnitus is a ringing, roaring, buzzing, or hissing in the ears or head that sometimes occurs with hearing loss.
Otosclerosis Risk Factors
Experts aren’t sure exactly what causes otosceloris, but they do know these risk factors may make you more likely to get it:
- Age: It usually starts when you’re young. You can develop otosclerosis between the ages of 10 and 45, but you’re most likely to get it during your 20s. Symptoms usually are at their worst in your 30s.
- Genetics: It often runs in families. About half of all people with otosclerosis have a gene that’s linked to the condition. But even if you have the gene, you won’t necessarily get it.
- Gender: Both men and women get otosclerosis. Women, though, have a higher risk. Experts aren’t sure why, but if you’re a woman and develop otosclerosis during pregnancy, you’re likely to lose your hearing faster than if you were a man or you weren’t pregnant.
- Race and Ethnicity: Caucasians are most likely to get it. About 10% develop otosclerosis. It’s less common in other groups and rare for African Americans.
- Medical History: Certain medical problems can raise your chances of otosclerosis. For example, if you had measles at any time, your risk may go up. Stress fractures to the bony tissue around your inner ear also might make it more likely to happen. And immune disorders, in which your immune system mistakenly attacks parts of your body, also can be linked to the condition.
How is otosclerosis diagnosed?
Otosclerosis is diagnosed by health care providers who specialize in hearing. These include an otolaryngologist (commonly called an ENT, because they are doctors who specialize in diseases of the ears, nose, throat, and neck), an otologist (a doctor who specializes in diseases of the ears), or an audiologist (a health care professional trained to identify, measure, and treat hearing disorders). The first step in a diagnosis is to rule out other diseases or health problems that can cause the same symptoms as otosclerosis. Next steps include hearing tests that measure hearing sensitivity (audiogram) and middle-ear sound conduction (tympanogram). Sometimes, imaging tests—such as a CT scan—are also used to diagnose otosclerosis.
How is otosclerosis treated?
Currently, there is no effective drug treatment for otosclerosis, although there is hope that continued bone-remodelling research could identify potential new therapies.
Otosclerosis can be treated surgically in a procedure known as a stapedectomy, where a surgeon inserts a prosthetic device into the middle ear to bypass the abnormal bone and permit sound waves to travel to the inner ear and restore hearing.
Alternatively hearing aids are very successful in treating hearing loss due to otosclerosis as the cochlear is generally functioning normally. It is important to discuss these options with an audiologist and ENT specialist to clarify potential risks and limitations of the operation and to determine which is the best course of action for you.
