OTITIS MEDIA
What Are The Types, Treatment & Management?
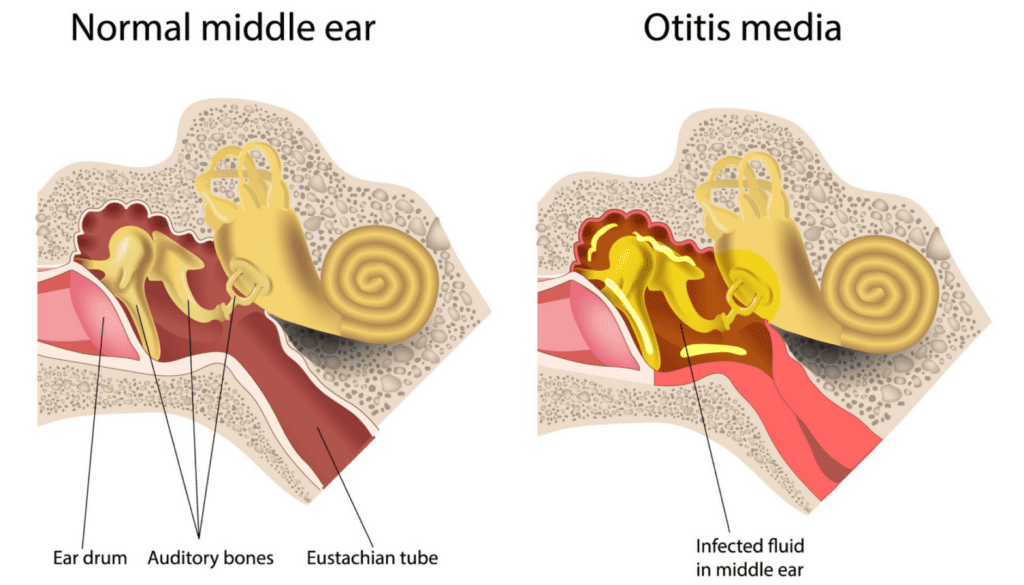
Otitis (ear) media (middle) is an infection of the middle ear cavity.
Otitis media can be divided into 3 types:
1. Acute Otitis Media
(AOM)
Otitis media usually starts with a cold or a sore throat caused by bacteria or a virus. The infection spreads through the back of the throat to the middle ear, to which it is connected by the eustachian tube. The infection in the middle ear causes swelling and fluid build-up, which puts pressure on the eardrum.
The middle ear infection occurs abruptly causing swelling and redness. Fluid and mucus become trapped inside the ear with symptoms including fever and ear pain. Sometimes the ear drum will rupture causing discharge from the ear and a noticeable reduction in discomfort.
The underlying cause can be viral, bacterial or both in combination. Bacterial causes can include Streptococcus pneumoniae, Haemophilus influenza and Moraxella catarrhalis.
2. Chronic Suppurative Otitis Media (SOM)
This is defined as a chronic discharging otitis media, often presenting with a copious, non-painful, white, yellow or green discharge, with no evidence of ear canal inflammation. It is often difficult to treat and if not of a very recent onset, usually contains multi-resistant organisms such as Pseudomonas or Proteus species.
3. Otitis Media with Effusion
(glue ear)
Glue Ear is a condition often without noticeable symptoms apart from minor hearing loss, in which there is fluid build up in the middle ear behind the ear drum. More about Glue Ear
Diagnosis
Diagnostic criteria for acute otitis media include rapid onset of symptoms, middle ear effusion, and signs and symptoms of middle ear inflammation. Fever, otalgia, headache, irritability, cough, rhinitis, listlessness, anorexia, vomiting, diarrhea, and pulling at the ears are common, but nonspecific symptoms. Hearing loss due to middle ear occlusion will also often be present and would require audiological assessment.
Whilst observation is an acceptable option in healthy children with mild symptoms, detection of middle ear effusion by otoscopy and tympanometry are key to establishing the diagnosis.
Risk Factors
- Low socio-economic status
- Ethnicity
- Immunocompromised
- Down syndrome
- Attending day care.
- Age: being between 6 and 36 months old
- Using a pacifier
- Being bottle fed instead of breastfed (in infants)
- Drinking while laying down (in infants)
- Exposure to cigarette smoke or high levels of air pollution
- Experiencing changes in climate and altitude
- Having had a recent cold, flu, sinus, or ear infection
Treatment and Management
- First line management of acute otitis media is analgesia to reduce the discomfort. Paracetamol alone is sometimes inadequate and Ibuprofen has been known to be more effective. Medical advice from your GP is recommended.
- Oral antibiotics will often only be used initially in high risk children or in persistent cases. Amoxycillin is indicated as an appropriate first line choice, for a 5 day course. Macrolide antibiotics, clindamycin, and cephalosporins are alternatives in penicillin-sensitive children and in those with resistant infections.
- Chronic suppurative otitis media is generally treated with antibiotic ear drops. Topical antibiotics have been shown to be most effective, and usually ciprofloxacin drops are used, for a maximum of 2 weeks. Dry ear toilet with tissue spears can be used, or the patient can lie on their side with the affected side down, prior to the eardrops. A common more effective toilet is using a 1:20 Betadine solution irrigation via a syringe, followed by drying with a tissue spear.
- For severe cases with perforation, surgical tympanoplasty (repairing the eardrum with a graft) may be required.
- For chronic cases audiological and language evaluations are recommended. Patients who do not respond to treatment should be reassessed. Hearing and language testing is recommended in children with suspected hearing loss or persistent effusion for at least three months, and in those with developmental problems.
